Table of Contents
What is Lyme Disease?
Definition and Overview
Lyme disease is an infectious disease caused by the bite of an infected tick, primarily the black-legged tick, also known as the deer tick (Ixodes scapularis). The disease is caused by the bacterium Borrelia burgdorferi and, in some cases, Borrelia mayonii. It is characterized by a combination of early symptoms1 that may include fever, headache, fatigue, and a distinctive skin rash called erythema migrans. If left untreated, the infection can spread to the joints, heart, and nervous system, leading to more severe health issues.
The global rise in Lyme disease cases has been attributed to several factors, including climate change, which affects tick populations and their habitats, as well as increased outdoor activities that enhance exposure to tick habitats. Understanding Lyme disease is crucial for effective prevention, early diagnosis, and treatment.
History of Lyme Disease
The recognition of Lyme disease as a distinct clinical entity began in the 1970s in Lyme, Connecticut, where a cluster of cases with similar symptoms was reported. Researchers identified the disease and its causative agent, leading to its classification in the early 1980s. Since then, the incidence of Lyme disease has increased significantly in North America and Europe, leading to ongoing research into its transmission, ecology, and treatment.
Historical data indicate that Lyme disease has likely existed for centuries, but the identification of its vectors and transmission dynamics has only recently come to light. Efforts to raise awareness and improve diagnostic methods have evolved alongside the increasing prevalence of this disease.
Causes of Lyme Disease
Transmission Methods
Lyme disease is predominantly transmitted through the bite of infected ticks2. These ticks are often found in wooded and grassy areas, which are their natural habitats. The transmission occurs when a tick feeds on the blood of a host, usually during the larval or nymph stages, which are most active in spring and summer. The tick must be attached for 24 to 48 hours for the transmission of the bacterium to occur, making prompt tick removal essential for prevention.
Besides ticks, there is ongoing research into other potential transmission routes, including blood transfusions and transplacental transmission during pregnancy, although these methods are considered rare. Understanding these transmission methods is vital for developing effective prevention strategies3.
Risk Factors
Several risk factors can increase a person’s likelihood of contracting Lyme disease. These include geographical location, as certain areas have higher tick populations and thus a greater incidence of Lyme disease. Individuals who spend significant time outdoors, particularly in wooded or grassy areas, are at a greater risk.
Additional risk factors include seasonal variations, with spring and summer being peak times for tick activity, and the presence of pets, which can carry ticks into homes. Awareness of these risk factors can help in implementing preventive measures to minimize exposure to ticks.
Who is More Likely to Get Lyme Disease?
Demographics
Lyme disease can affect individuals of any age, gender, or ethnicity4, but certain demographics show higher susceptibility. Children are particularly vulnerable due to their outdoor play habits, while adults who engage in outdoor recreational activities, such as hiking and camping, are also at increased risk. Studies have shown that males tend to have a higher incidence of Lyme disease compared to females, potentially due to increased outdoor exposure.
Moreover, those with weakened immune systems or underlying health conditions may experience more severe manifestations of the disease, emphasizing the need for awareness and preventive strategies among vulnerable populations.
Environmental Factors
Environmental factors, such as climate and habitat, play a significant role in the prevalence of Lyme disease. Warmer temperatures and changing precipitation patterns affect tick populations and their habitats. Regions with a dense deer population often have higher rates of Lyme disease due to the deer being a primary host for adult ticks. Additionally, urbanization and land use changes can influence tick distribution, exposing more people to tick bites.
Public health officials and researchers continue to study these environmental influences to better predict and manage Lyme disease outbreaks, contributing to more effective prevention strategies.
Symptoms of Lyme Disease
Early Symptoms
The initial symptoms of Lyme disease often appear within three to 30 days after a tick bite. The hallmark of early Lyme disease is the characteristic bull’s-eye rash, known as erythema migrans, which appears at the site of the tick bite. This rash is typically red, circular, and may expand over time. Other early symptoms may include fever, chills, fatigue, headache, muscle and joint aches, and swollen lymph nodes.
Recognizing these early symptoms is critical, as prompt treatment can prevent the progression of the disease. Early intervention often results in a full recovery without lasting effects, highlighting the importance of awareness and education regarding Lyme disease symptoms.
Late Symptoms
If Lyme disease is not treated in its early stages, it can lead to more severe health complications. Late symptoms may develop weeks to months after the initial infection and can affect the joints, heart, and nervous system. Symptoms may include severe joint pain and swelling, particularly in the knees, and neurological issues such as meningitis, Bell’s palsy, or peripheral neuropathy.
Individuals may also experience cardiac problems, including Lyme carditis, which can cause heart palpitations and dizziness. The progression to these late-stage symptoms underscores the necessity for timely diagnosis and treatment to prevent long-term complications.
How is Lyme Disease Diagnosed?
Diagnostic Criteria
Diagnosing Lyme disease can be challenging due to its nonspecific symptoms and the overlap with other illnesses. Healthcare providers typically rely on a combination of clinical evaluation and patient history, including potential exposure to ticks. The presence of erythema migrans can be a strong indicator, but not all patients exhibit this rash.
In addition to clinical criteria, the diagnosis may involve a two-tiered testing approach. The first tier includes enzyme-linked immunosorbent assays (ELISAs) to detect antibodies to the Lyme bacteria. If positive, a second-tier test, such as the Western blot, is performed to confirm the diagnosis. However, these tests may yield false-negative results, especially in early stages of the disease.
Laboratory Tests
Laboratory tests play a crucial role in the diagnosis of Lyme disease, particularly in cases where the clinical presentation is ambiguous. Serological tests are the most common method for detection, measuring the immune response to the bacteria. While these tests are useful, they are not definitive, and results must be interpreted in conjunction with clinical findings and patient history.
In some cases, polymerase chain reaction (PCR) tests can be employed to detect the presence of the bacteria in fluid samples, such as blood or synovial fluid from inflamed joints. However, these tests are less commonly used due to their complexity and the need for specialized laboratory facilities.
Drug-Free Treatments for Lyme Disease
Natural Remedies Overview
While conventional treatments for Lyme disease typically involve antibiotics, many individuals seek natural remedies as complementary approaches or alternative treatments. Various natural substances are believed to have antimicrobial properties, support the immune system, and reduce inflammation associated with Lyme disease. It is essential to consult with healthcare professionals before starting any natural treatments to ensure safety and efficacy.
Natural remedies may vary widely in their effectiveness, and research is ongoing to validate their use. Patients should approach these treatments with caution and under guidance, particularly when dealing with a complex condition like Lyme disease.
Why do Antibiotics have limited use for Chronic Lyme disease?
- Borrelia is a stealthy, highly evasive micobe
- Borrelia has a very slow growth
- Borrelia becomes part of the microbiome
- Co-Infections of microbes complicate therapy
- Microbiome is disrupted by chronic antibiotic use
- The Immune system is disrupted by chronic use of antibiotics
- Antibiotics tend to damage the mitochondria of the cell
- Protective biofilms on the cell can get disrupted with antibiotics
Herbal Remedies
Herbs such as garlic, cat’s claw, and Japanese knotweed are often cited for their potential benefits in managing Lyme disease. Garlic is known for its antimicrobial properties and may help combat infections. Cat’s claw is used in traditional medicine for its anti-inflammatory and immune-boosting effects. Japanese knotweed contains resveratrol, which has been studied for its role in reducing inflammation and supporting cardiovascular health.
Additionally, tinctures and extracts of these herbs may be formulated to enhance their bioavailability and efficacy. However, the scientific evidence supporting their use in Lyme treatment is still limited, necessitating further research to establish guidelines for their application.
Dietary Considerations
An anti-inflammatory diet may help support recovery from Lyme disease. Emphasizing whole foods, such as fruits, vegetables, whole grains, and healthy fats, can promote overall health and bolster the immune system. Foods rich in antioxidants, such as berries and leafy greens, may help mitigate inflammation and oxidative stress associated with the disease.
Additionally, some individuals may choose to eliminate processed foods, sugar, and gluten, which can contribute to inflammation and may worsen symptoms. It is advisable to work with a nutritionist or healthcare provider to develop a diet tailored to specific health needs during recovery.
Immune Support Strategies
Supporting the immune system is crucial in the management of Lyme disease. Natural immune boosters, such as vitamin C, vitamin D, and zinc, play vital roles in enhancing immune function. Probiotics may also be beneficial, particularly for individuals undergoing antibiotic treatment, as they can help maintain gut health and balance the microbiome.
Stress management techniques, such as mindfulness, yoga, and meditation, can also support overall well-being and immune health. A holistic approach that addresses both physical and mental health can be advantageous in the recovery process from Lyme disease.
Can Lyme Disease Be Prevented?
Preventive Measures
Preventing Lyme disease primarily involves reducing exposure to ticks. Individuals are encouraged to wear protective clothing, such as long sleeves and pants when venturing into tick habitats. Using insect repellents containing DEET or picaridin can significantly reduce the risk of tick bites. Additionally, performing thorough tick checks after outdoor activities is essential to identify and remove ticks promptly.
Landscaping strategies, such as keeping grass trimmed and removing leaf litter, can also diminish tick habitats around homes. Public health initiatives focused on education and awareness play a crucial role in reducing the incidence of Lyme disease within communities.
Education and Awareness
Increasing awareness about Lyme disease is key to its prevention. Educational programs aimed at informing the public about tick biology, the risks associated with tick bites, and the importance of early detection and treatment have proven effective in reducing Lyme disease cases. Schools, parks, and community organizations can collaborate to disseminate information and resources to promote safer outdoor practices.
Public health campaigns emphasizing the need for preventive measures, such as tick checks, appropriate clothing, and the use of repellents, can empower individuals to take proactive steps against Lyme disease. The integration of education into community health initiatives can significantly impact the overall incidence of the disease.
Lyme Disease in Children
Symptoms and Diagnosis
Children may exhibit similar symptoms of Lyme disease as adults, including fever, headache, fatigue, and the characteristic rash. However, there are instances where children may experience atypical symptoms, such as behavioral changes or increased irritability, which can complicate diagnosis. Early recognition of these symptoms is crucial, as children may be at heightened risk for severe complications if the disease progresses untreated5.
Diagnosing Lyme disease in children involves careful evaluation of symptoms, potential tick exposure, and the presence of erythema migrans. Medical professionals may utilize serological testing to confirm the diagnosis. Given the often-overlapping clinical presentation with other childhood illnesses, a thorough assessment is essential for accurate diagnosis.
Treatment Options
Although Lyme disease is a bacterial infection that should be treated by a doctor using antibiotics, symptoms may be alleviated by natural remedies like herbal medicine. Natural treatments may also help with inflammation, detoxification, cellular repair, sleep, and your immune system, which is affected by Lyme disease.
Chronic Lyme disease patients frequently experience symptoms that make their everyday lives difficult, if not impossible. Following an immediate tick bite, antibiotics are usually an effective treatment for Lyme disease; however, some people experience persistent symptoms.
After receiving antibiotic treatment for Lyme disease, 10% of patients develop post-treatment Lyme disease syndrome. Furthermore, antibiotics may have adverse effects of their own. Others might never be aware that they were bitten by a tick and continue to suffer for years without receiving the appropriate diagnosis, which can lead to the disease becoming chronic if left untreated.
The treatment of Lyme disease in children typically involves a course of antibiotics, such as doxycycline or amoxicillin, depending on their age and specific circumstances. The duration of treatment may vary based on the severity of symptoms and any potential complications. While children tend to respond well to antibiotic treatment, ensuring adherence to the prescribed regimen is critical for successful recovery.
In conjunction with medical treatment, supportive care strategies, such as hydration and rest, can enhance recovery. Families are encouraged to remain vigilant and monitor for any persisting or worsening symptoms after treatment, as post-treatment Lyme disease syndrome may occur in some cases, necessitating further evaluation.
Lyme Disease in Teenagers
Symptoms and Diagnosis
Teenagers may experience Lyme disease symptoms similar to those seen in adults and children. Common symptoms include fatigue, fever, joint pain, and the characteristic rash. However, the potential for misdiagnosis is high due to the commonality of symptoms with other teenage health issues, such as stress or viral infections. Awareness among teenagers and their parents regarding the signs of Lyme disease is crucial for early intervention.
The diagnostic process for teenagers follows similar protocols, including a review of symptoms and potential exposure to ticks. The presence of erythema migrans is a strong indicator, but serological testing may also be employed when necessary. It’s essential for healthcare providers to conduct a comprehensive evaluation to differentiate Lyme disease from other conditions.
Treatment Strategies
Teenagers diagnosed with Lyme disease typically receive a course of antibiotics, similar to other age groups. The standard treatment regimens are generally effective, and most teenagers recover fully with proper medical management. Patients are encouraged to discuss any concerns regarding treatment, such as potential side effects or treatment duration, with their healthcare provider.
In addition to antibiotic therapy, holistic approaches, including lifestyle modifications and dietary adjustments, can offer supplementary support during recovery. Engaging in discussions about health and wellness can empower teenagers to take proactive roles in their recovery and long-term health.
Conclusion
In summary, Lyme disease is a complex and multifaceted condition that requires a thorough understanding of its symptoms, causes, and treatment options. Through education and awareness, individuals can take proactive steps to reduce their risk of infection. Natural remedies, alongside traditional treatments, can offer additional support for those affected by Lyme disease. Understanding the unique aspects of Lyme disease in both children and teenagers is essential for timely diagnosis and effective management.
FAQs about Lyme Disease
What are the early signs of Lyme disease?
Early signs include fever, chills, fatigue, headache, muscle and joint aches, and the characteristic erythema migrans rash.
Can Lyme disease be transmitted through pets?
While pets can carry ticks, Lyme disease is primarily transmitted through tick bites directly to humans.
How long does it take for Lyme disease symptoms to appear?
Symptoms typically appear within 3 to 30 days after a tick bite.
Is Lyme disease curable?
Yes, Lyme disease is treatable with appropriate antibiotics, especially if caught early.
What should I do if I find a tick on my body?
Remove the tick as soon as possible using a tick removal spoon or fine-tipped tweezers, grasping it as close to the skin’s surface as possible. Clean the bite area and monitor for symptoms.
Products
At Home Tests
-
←→
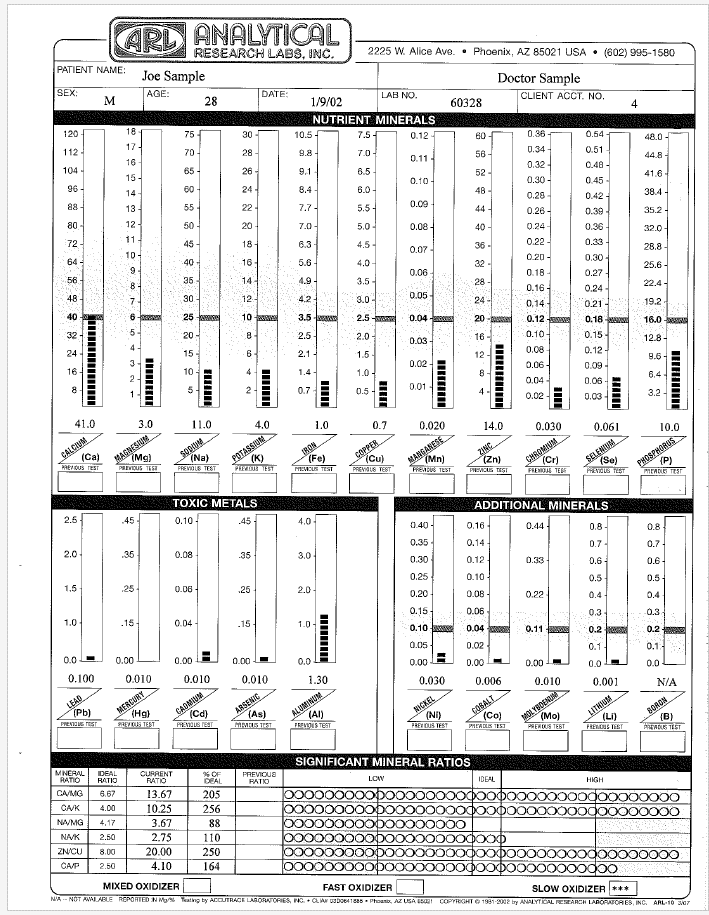
Analytical Research Labs Hair Test
$179.00$149.00Providing a mineral blueprint of one’s biochemistry, an Analytical Research Labs Hair Minerals Test reports levels of minerals and heavy metals in your body giving possible reasons for your symptoms, with suggestions for nutritional supplements and diet changes. Hair tissue mineral analysis can provide pertinent information about balanced nutrition, one’s metabolic rate, energy levels, sugar and carbohydrate tolerance, stage of stress, immune system and glandular activity.- Buy 2 at $145.00
Analytical Research Labs Hair Test
$179.00 $149.00Successfully Added to your Shopping CartAdding to Cart... -
←→
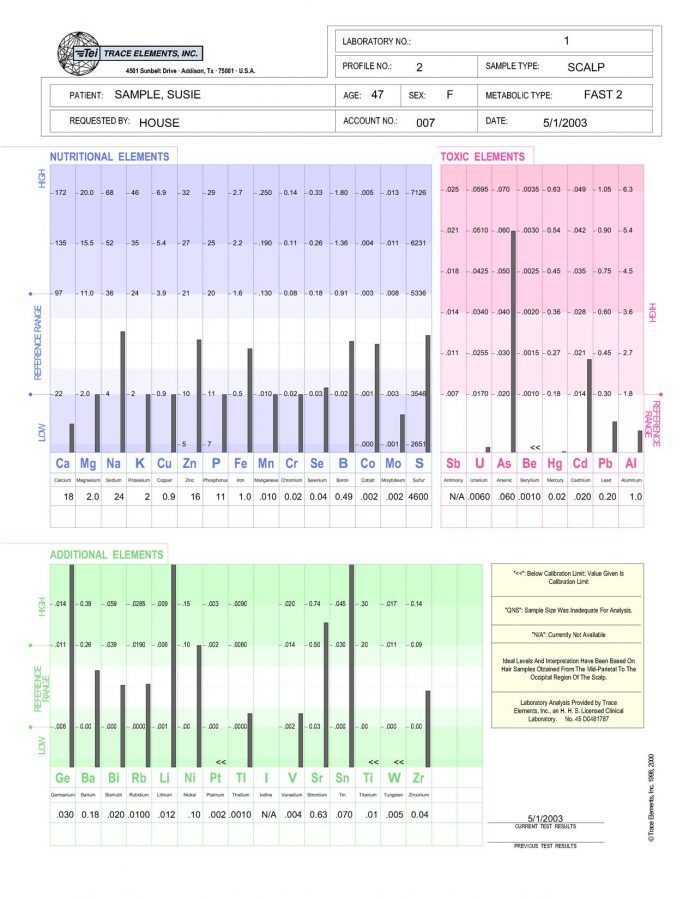
Trace Elements Nutritional Deficiencies Hair Test
Nutritional Tests, At Home Health Tests, Toxic Metals Tests, Hair Tests, Autism Tests, Immune System Tests$188.00 $148.00Successfully Added to your Shopping CartAdding to Cart... -
←→
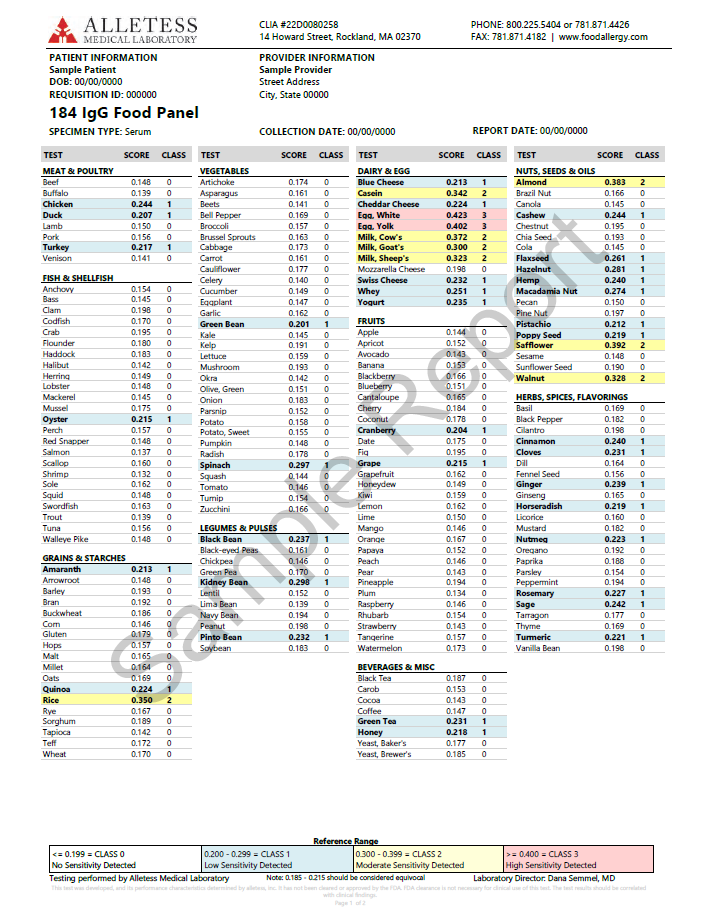
Alletess Food Allergy Sensitivity Test
$269.00$223.00Food sensitivities may be causing many of your health issues. Test now with this convenient at home test; no lab visit required.Alletess Food Allergy Sensitivity Test
At Home Health Tests, Allergy Tests, Blood Spot Tests, Allergy Solutions, Lung Solutions, Gastrointestinal Solutions$269.00 $223.00Successfully Added to your Shopping CartAdding to Cart...
Supplements
Lyme Supplements Package 
-

Lyme Combo Package
$374.91$357.90This is a package of supplements specifically designed for the Lyme patient- Buy 2 at $340.00
Maximum quantity exceededMinimum purchase amount of 0 is required -
←→
Calcium 2-AEP
Supplements, Mineral Supplements, Muscle Solutions, Anxiety, Stress, Depression Solutions, Bone Solutions$14.40Successfully Added to your Shopping CartAdding to Cart... -
←→
Buffered C with Calcium, Magnesium & Potassium
Supplements, Vitamin Supplements, Skin Solutions, Cancer Solutions, Immune System Solutions, Antioxidant Supplements, Allergy Solutions, Autism Solutions$11.70Successfully Added to your Shopping CartAdding to Cart... -
←→
Calcium Orotate
Supplements, Mineral Supplements, Bone Solutions, Nerve Damage Solutions, Skin Solutions, Heart Solutions$26.80Successfully Added to your Shopping CartAdding to Cart... -
←→
Selenium
Supplements, Mineral Supplements, Heart Solutions, Immune System Solutions, Hormone Solutions, Antioxidant Supplements$13.10Successfully Added to your Shopping CartAdding to Cart... -
←→

Zinc Aspartate
$6.00Zinc AspartateMaximum quantity exceededMinimum purchase amount of 0 is requiredZinc Aspartate
Supplements, Mineral Supplements, Skin Solutions, Bone Solutions, Hormone Solutions, Immune System Solutions, Gastrointestinal Solutions$6.00Successfully Added to your Shopping CartAdding to Cart... -
←→

Lithium Orotate
Supplements, Mineral Supplements, Autism Solutions, Nerve Damage Solutions, Immune System Solutions, Gastrointestinal Solutions$16.30Successfully Added to your Shopping CartAdding to Cart...
References
- Centers for Disease Control website. Lyme disease. www.cdc.gov/lyme/. Updated May 15, 2024. [CDC] ↩︎
- How is Lyme Disease Transmitted? [Hartford County Health Department] ↩︎
- Not bitten by Ixodes Tick or bitten without symptoms, Why still worry? [NIH] ↩︎
- Age- and Sex-Specific Differences in Lyme Disease Health-Related Behaviors, Ontario, Canada, 2015-2022 [NIH] ↩︎
- Signs and Symptoms of Untreated Lyme Disease [CDC] ↩︎
- http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L631138166
- https://doi.org/10.3389/fmed.2017.00169
- https://doi.org/10.1155/2017/3026370
- https://doi.org/10.1016/j.ctim.2018.03.010
- https://doi.org/10.1016/j.ejmech.2017.03.004
- https://doi.org/10.1016/j.phymed.2009.10.013
- https://doi.org/10.1007/PL00000268
- https://doi.org/10.1089/acm.2014.0127
- https://doi.org/10.1016/j.mehy.2017.06.015
- https://doi.org/10.1155/2014/978582